Just over two months since ‘Freedom Day’ and in many places it feels like Covid-19 is a distant memory. Masks have been abandoned, schools are ‘back to normal’, people are crowding back on tubes; meanwhile you still can’t go into a vet’s consulting room with your pet. So where exactly are we with regards to Covid-19 in England?
I’m going to try and tackle some of the questions I get asked regularly.
I’ve met people who have been double jabbed who have caught Covid-19 and become very unwell. Is it really true that the vaccines protect against severe illness?
Yes, the vaccines do work really well in protecting us against severe disease and death, but they are not an impenetrable barrier against Covid-19. They give your body a head-start in knowing how to fight the virus, should you get exposed. But everyone’s immune system is different, and although you have primed it with the vaccine, it may still take a little longer to ramp up its attack, giving the virus more of a chance to spread and cause symptoms. However, without the vaccine, your body would be having to learn how to fight after the infection has already taken hold, giving itself a much harder job.
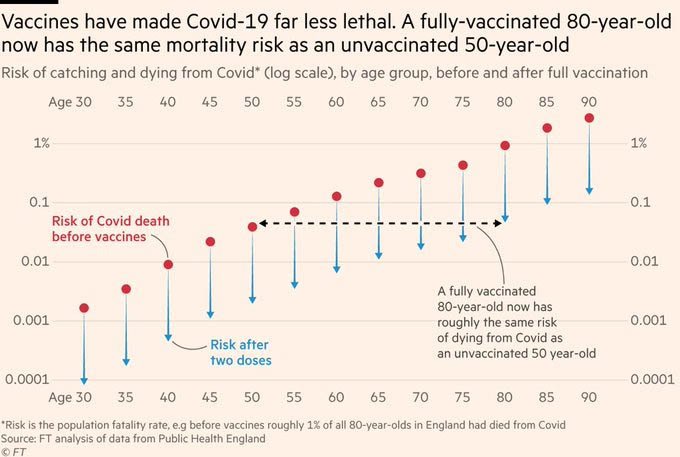
The data from the original trials, which have been replicated many times in numerous studies looking at numbers in the real world, showed that two doses of a Covid-19 vaccine reduces the risk of getting severe illness or dying from Covid-19 by about 90 per cent (numbers vary but they are generally between 85 and 95 per cent). The risk reduction percentage applies to you personally, so if you were high risk before vaccination you remain so relative to the population at large, BUT the reduction in your risk will still be really significant.
As you can see, the vaccines greatly lower your risk of getting very ill or dying from Covid-19, but they don’t eliminate the risks altogether.
Are the vaccines wearing off?
There does seem to be some evidence of vaccines’ efficacy starting to wane, but there is a LOT of uncertainty over this, as you can imagine, with new data coming in as time goes on.
The most recent data from Public Health England finds that there is some decrease in protection against hospitalisation in the over 65s and those who are clinically extremely vulnerable, but less of a decrease in the under 65s. However, even in those groups with the biggest decrease in immunity, the vaccines are still giving around a 70 per cent reduction in risk, so protection remains high.
Third jabs should help give the immune systems in those more vulnerable groups another boost, but at the moment it looks like the vast majority of people will not need a booster just yet.
I’ve heard most people in hospital with Covid-19 are double jabbed. Doesn’t that mean the vaccines aren’t working?
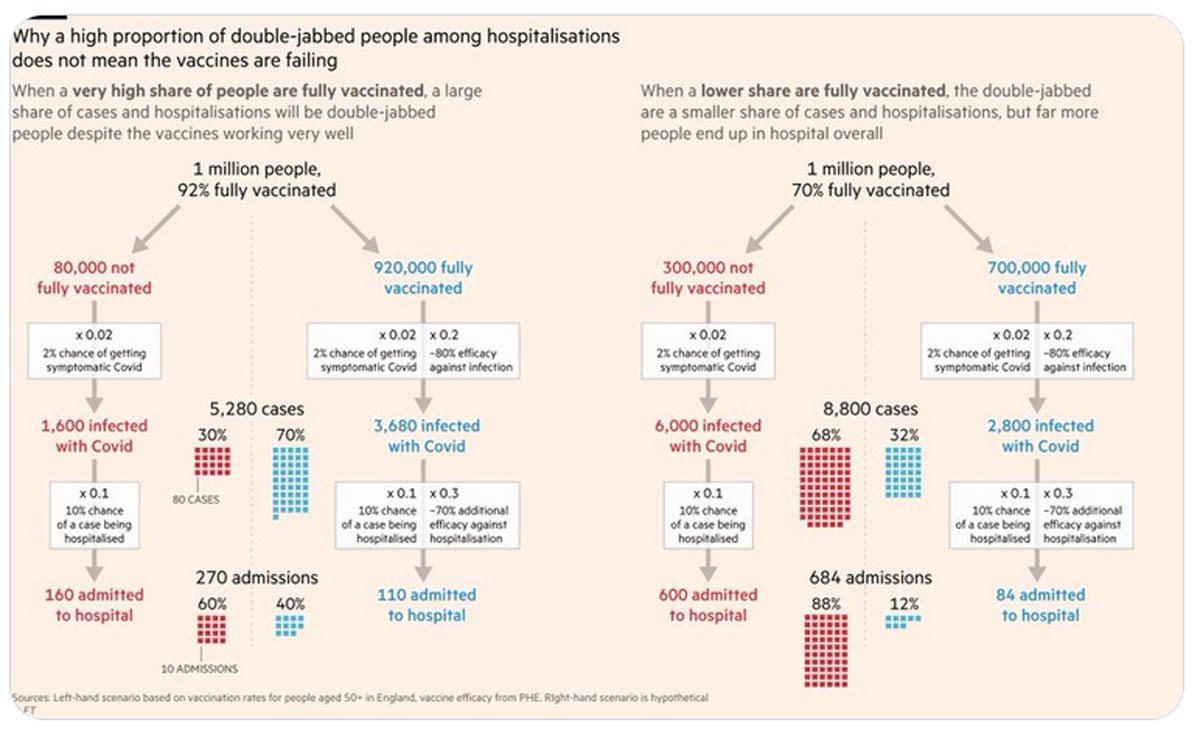
In order to understand why the hospitals are full of vaccinated people, we need to look at what is going on in the population. If 100 per cent of the population was vaccinated, then you would expect 100 per cent of all the hospital admissions to be vaccinated. In the same way, most people who end up in hospital after a car crash were wearing seatbelts. That doesn’t mean that seatbelts don’t work, its just an indication that the vast majority of people wear seatbelts!
So the reason why the majority of people in hospital with Covid have been vaccinated is because the vast majority of the population, and especially the population most vulnerable to Covid-19, have been vaccinated.
The maths is explained graphically here.
Around 15 per cent of the over 70’s being admitted to hospital with Covid-19 are unvaccinated, despite only five per cent of that population being unvaccinated.
If I can still catch and transmit Covid-19 when I’m vaccinated, what is the point in getting the vaccine if I am not vulnerable?
There has been a lot of mixed messaging around whether you can still catch and transmit Covid-19 if you are vaccinated. The original trials only looked at the reduced risks of severe disease and death, and early public health messaging was to remain cautious following vaccination, as we knew people could still catch Covid-19 and, therefore, there was still a risk of transmitting it to others.
However, over the last 6 months there have been numerous studies using real world data that show that being vaccinated not only reduces your risk of getting infected by between 65 and 95 per cent, but it also reduces your risk of transmitting it to others. This appears to be because infections in vaccinated people involve lower levels of virus, and they tend to be ill for a shorter time. One study showed how the unvaccinated were likely to be contagious for many more days than those who were vaccinated, if they became infected.
The UK Covid Vaccine Surveillance Report provides a good review of all the data available on how well vaccines work to protect against infection, infection with symptoms, hospitalisation and death, as well as early data on protection against spreading Covid to others:
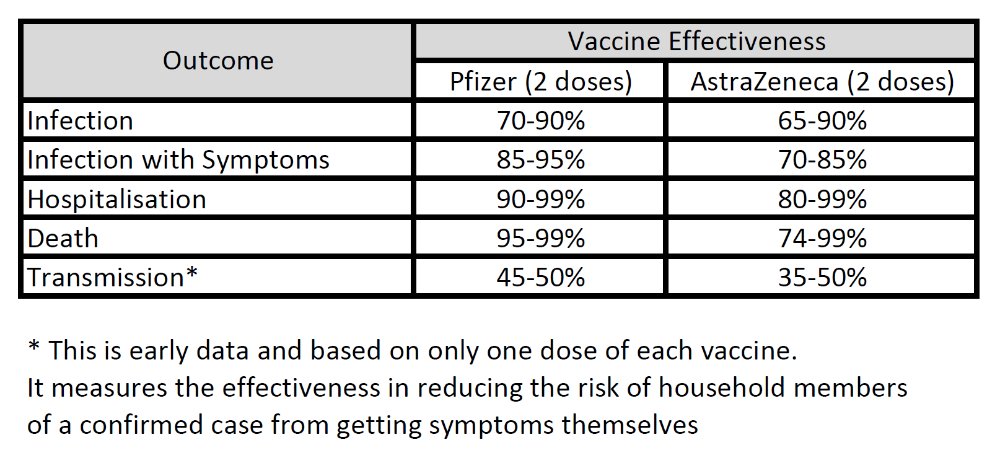
So yes, getting vaccinated does actually protect those around you, as well as yourself. You are less likely to get a Covid-19 infection in the first place, and if you do become infected, you will be less contagious.
Do the vaccines work against the variants as well as they did against the original strain?
As @sailorrooscout (a great vaccine scientist to follow on twitter if you are into that sort of thing!) succinctly puts it, there is yet to be a variant that isn’t susceptible to the vaccines.
There has been some evidence to suggest that the vaccines, particularly AstraZeneca, were not as affective against the Beta variant, but they still provided some level of protection. Fortunately, for the Delta variant, which is now the most dominant worldwide, the vaccines are holding up really well. Both the AstraZeneca and Pfizer vaccines have been shown to provide more than 90 per cent protection against hospitalisation following a Delta Covid infection.
The reason many vaccine scientists are reasonably confident that the vaccines will continue to hold up well is that the vaccine targets the part of the virus that enables it to enter and infect cells. If that part changes so much that antibodies no longer recognise it, the change is also likely to mean the virus is no longer able invade cells. This is by no means a certainty, but it seems to be a reasonably likely outcome.

England has given up on masks in public spaces including schools and shops. Does that mean masks don’t really matter?
We are fairly isolated in our attitude to masks in this country! Masks are still required in most of the rest of the world. Here in the UK, it was decided back in July that people could make up their own minds about whether or not they felt the need to wear a mask. Unfortunately, that policy seems to have fundamentally missed the point of masks, which is to protect those around you. Mask wearing is a really cheap and simple means of limiting the spread of Covid-19 and I urge everyone to continue wearing one when out in public in indoor spaces.
There has been plenty of evidence showing that masks are effective, which I covered in a previous article, but more recently there was a large scale randomised trial into mask wearing which concluded that mask wearing reduced symptomatic Covid-19 infections. Another study in Arizona showed that Covid-19 outbreaks were almost four times more likely in schools that did not mandate mask-wearing compared with those that did.
Will there be a big surge in cases as universities go back like there was last year?
Nothing is certain, but the general feeling amongst scientists is that there is unlikely to be the same sort of spike in cases as we saw last year. Most university students have now had the vaccine. They are also an age group who have likely been mixing more than others in previous months, making them more likely to have been exposed to the virus already.
Data from Yale University is looking good. They have a very high level of vaccination (99.4 per cent of undergraduates, 97.8 per cent of graduates, 95.1 per cent of faculty, and 92.5 per cent of staff), have maintained masks, are holding in person teaching, and have had only three positive cases in the last week. This shows what can be achieved in a university environment and hopefully UK universities will follow a similar pattern.
Are the vaccines safe in children? When will my child be able to get one?
Yes they are safe, and hopefully soon (if your child is 12-15 years old)!
To date, 54 per cent of 12-15 year olds in the US (over eight million kids) have received at least one dose, as have 79 per cent in Spain, 68 per cent in France and good percentages in many other European countries. Millions of children have received the vaccine with very little in the way of serious side effects. I won’t go into detail here as I have a full article on the subject that I wrote a couple of weeks back.
It seems as if the vaccine rollout for 12-15 year olds will be happening through schools, so if you haven’t heard yet, check with your school when they are likely to be doing them.
Pfizer has recently completed their trials into vaccinating 5-11 year olds, and found the vaccine to be safe and to work well. They have submitted their findings to the FDA in the US, so we will have to wait and see if it gets approval.
Should I be worried about Long Covid? – some people say it’s no big deal and others seem really concerned.
We have known for many years that viruses can trigger long-lasting side effects, and Covid-19 is no different. The full extent of the long term effects of a Covid-19 infection will not be known for a while, but it is a virus that can target almost any organ in your body and there is evidence that it can lead to long term changes in the heart, lungs and even the brain.
Millions of people are currently suffering from Long-Covid, where they continue to experience symptoms such as fatigue, muscle aches, brain fog, and headaches for many weeks or months. This can be debilitating and should never be treated lightly.
There have been several studies into Long Covid in children, including one from Kings College London, based on parents reporting their children’s symptoms using the Zoe Covid-19 app. It found around one in 20 children still had symptoms after 28 days and one in 50 still had symptoms after eight weeks. Another study from UCL and PHE, based on questionnaires sent to children who tested positive for Covid-19, found that as many as one in seven children still had symptoms after 15 weeks. Whether the numbers are as high as one in seven or as ‘low’ as one in 50, that is an awful lot of children suffering long term health problems from catching a disease that they could have been protected from.
A recent ONS analysis suggests nearly a million people in the UK (1.5 per cent of the entire population) were experiencing Covid-19 symptoms more than 4 weeks after infection – that is to say, one million on a given day, currently. It’s not just that one million have had Long Covid at some point during the pandemic. Also, 40 per cent of those still experiencing symptoms were infected more than a year ago.
Long Covid is very real; it is affecting people’s day to day lives, and no-one knows how long it will last. People can argue about how often it occurs, and different studies will have differing results, but even the lowest estimates look set to leave us with a huge future health-care burden, not to mention hardship for the sufferers
Don’t we just need to learn to live with Covid-19, like we do with flu?
There are different meanings to the term “learning to live with Covid-19”. To some it means pretending Covid-19 has disappeared and everyone going back to living and behaving as they did before the pandemic hit. Obviously, we would all love to be able to do that! But if you chose to swim in a tankful of sharks and they keep eating parts of your body, you aren’t “learning to live with the sharks”, you are being eaten alive! Ignoring Covid-19 and wishing it would go away is not a sensible, or effective, method for moving forwards. It will inevitably lead to thousands of avoidable deaths, and hospitals continuing to struggle to treat both Covid-19 patients, and all the other patients they are trying to see.
A better interpretation, and one we can see in action in Yale University as mentioned above, is working out what measures we need to keep in place to allow us to go about our daily lives relatively freely, while also keeping infection rates low. This involves a combination of high vaccination rates, mask-wearing in crowded spaces, keeping your distance where possible and financial help for infectious people so they can isolate without worrying about their income. This is largely what is happening in continental Europe, where they are managing to keep their case numbers much lower than we are in the UK, while still going about their ‘normal’ lives.
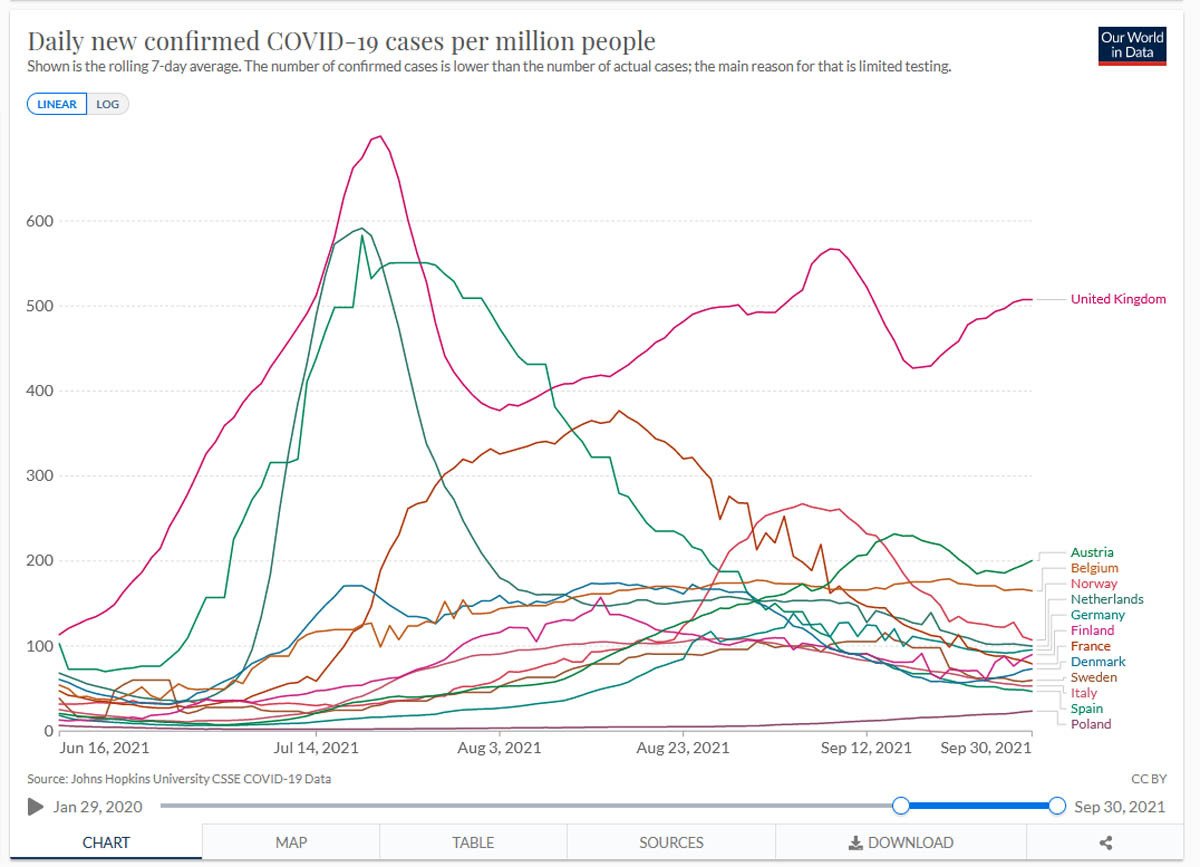
Hospital admissions and confirmed Covid-19 deaths show a similar pattern, with the UK having much higher numbers than our European counterparts.
Meanwhile, in England, children have gone back to schools ‘as normal’ with no masks, distancing, ventilation, bubbles or isolations for contacts etc. As a consequence, over 100,000 children were off school last week with either confirmed or suspected Covid-19, higher than at any other time during the pandemic. To me this isn’t “learning to live with it”.
As for comparisons with flu? We know that Covid-19 is NOT the same as flu. It is many times more infectious and kills a much higher proportion of people than flu does. It may eventually evolve to become less deadly (although that is not a certainty), and as more people get vaccinated, it will be less able to spread. We may be able to keep levels low with yearly boosters as we do with flu, but we aren’t there yet and certainly shouldn’t behave as if we are.
No one can predict what the future will bring, but if Covid-19 has taught us anything, it is that hoping for the best and not planning for the worst doesn’t play out well.