
The Covid Inquiry is due. The prime minister will no doubt try and dodge it. I am going to post on one major pandemic mistake a few times a week until we get that inquiry. I will focus on mistakes relating to clinical care or impact on health systems. You can judge how this government has done!
There are three basic tenets to an infectious disease outbreak:
1. Find the sick
2. Treat the sick
3. Stop others getting sick.
Looking at the first aspect, and specifically TRIAGE – finding the sick!
Why did we leave so many at home?
Triage.
Triage has different meanings. Both apply here. The first type of triage is to carry out a brief assessment and try and categorise how serious the problem may be. Often this leads to a triage disposition – how soon is a full assessment required and who should do it?
This is what happens each time you go to Accident and Emergency: a brief assessment with your pulse, temp, oxygen levels, etc…and a chat with (usually) a nurse, who then makes the call: see straight away, see within an hour, etc…(it’s actually colour coded usually). GPs do the same everyday.
The second type of Triage applies to critical incidents, where large numbers of patients are expected. This focuses on utilising limited resources to save the most lives. Typically, this form of triage is undertaken by the most senior clinician- GP or Consultant or an advanced nurse practitioner.
The World Health Organisation (WHO) guidelines on triage for Covid were as expected. Anyone with symptoms of Covid should be CLINICALLY assessed, tested, and (at least for most of 2020) admitted to appropriate level of care. Field hospitals for low risk, low severity, and hospital for higher risk/severities.
The UK and US (and a few other countries) took a different approach. The order was to stay at home and only contact healthcare providers if the illness became severe.
Both countries deployed the use of online, automated triage systems. I will explain…
In the U.K., the guidelines issued in March 2020 advised the public – only if worried – to use “111 Coronavirus Symptom Checker” instead of contacting GPs or calling 111. This was an online platform where the member of public entered their symptoms and answered some set question
…the computer algorithm then decided what level of care you need: call 111, see GP, go to the Emergency Department, call an ambulance.
Be clear, the questionnaires were not reviewed by anyone. The algorithm had set criteria and set thresholds for advising onward care.
Other countries employed symptom checkers as an extra tool – questionable in itself. But the UK was entirely UNIQUE in using the symptom checkers as the primary point of triage. It had never been done before – a major incident being triaged by an automated system.
How did it perform?
There are a number of cases put forward by @CovidJusticeUK and reported in coroners’ reports of delayed access to treatment using the 111 system.
We also studied it….
https://informatics.bmj.com/content/28/1/e100187
…we compared symptom checkers across four countries by simulating typical Covid cases and, importantly, cases that looked like Covid but were actually something else very serious (e.g. pneumonia and sepsis).
Our results were published in the BMJ Health and Care Informatics.
Results:
Both the US and U.K. triaged in fewer than half the cases that the Singapore and Japanese symptom checkers did. More worrying, they consistently missed severe Covid and pneumonias – advising such cases to stay home with no follow-up AT ALL!!
I was utterly shocked when the results came in. Indeed, so concerned that I released the data immediately to NHS Digital and contacted the clinical team there. As it stood…you could be 85 years old, with multiple co-morbidities, fever and cough for seven days and “stay home” with no follow-up!
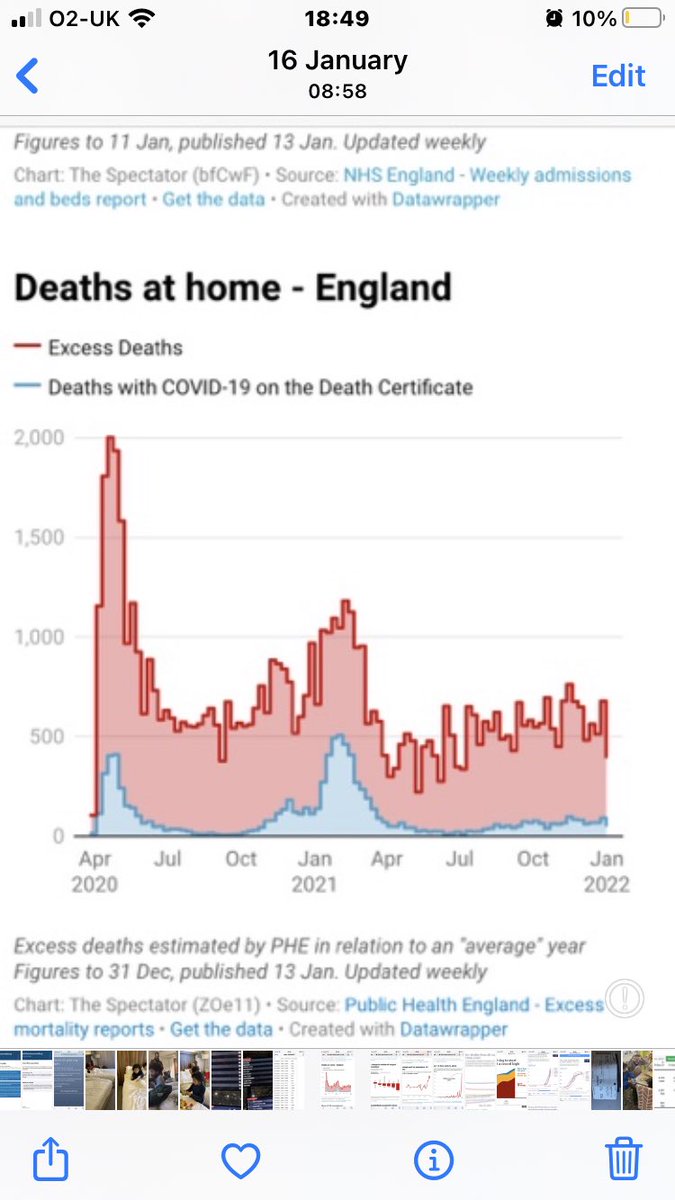
My issue was, of course, patient safety. Delaying intervention increases the chance of death and disability. And people were dying at home. A lot of people.
There was also the issue of effective use of hospital resources. Delayed presentation meant higher and longer care needs!
The entire NHS survives because our incredible GPs are so good at telling when someone needs hospital care (of course they don’t always get it right, but they are very good). Intervention early = short admission and low complications. Late also = filling hospitals up sooner!
The clinical team at NHS Digital were very engaged, looking to improve the algorithm. We had a meeting and they took our results. Next I hear in May 2020, they were discussing it with senior advisers/executives.
Eventually our results were published and picked up by MSM.
The BBC questioned NHS Digital, who simply stated that our results were dated and referred to an old version of the 111 triage system.
So, we repeated the study…
https://www.bbc.co.uk/news/health-56323915.amp
There were some improvements. For example, breathing issues typically led to contact of some sort.
But, the UK 111 and US CDC symptom checkers remained dangerous.
Notably, there is also serious concerns that they actually increase demands on healthcare!
https://informatics.bmj.com/content/28/1/e100448.info
Crucially, the 111 online patient-led triage system remained central to the UK response. The public were actively discouraged from contacting GPs or going directly to A&E.
Instead of clinical triage, the UK population received automated triage or no triage at all.
An important Covid inquiry question?
Absolutely!
Triage is so central to our response. Done badly it will increase death and disability. Done well and it saves lives and resources.
To this day, we have seen no quality or safety data/assessments about these triage systems.
Questions:
- What were the considerations that led to the lower standard of triage for Covid patients?
- Was it known that the elderly and vulnerable would be exposed to greater risk with such a triage system?
- And why was primary care displaced from the pathway to later in the pathway?
- And crucially, did the resources exist to clinically triage all cases? That is, was care rationed and compromised prematurely?
We know there was “capacity” within the NHS during the first wave, and probably others. Why was the entire nation triaged as if there were none?
Be clear, GPs and hospitals had no say on these triage systems. Our bit came after the automated 111 triage. Why such high barriers for assessment? Could manpower have been moved around to provide actual clinical triage? Likely!
We deserve to know for clarity, but it is more crucial to identify the faulty processes that led to such a seemingly untested online triage system replacing usual standards of care.
Future pandemic responses depend on admitting where it went wrong and correcting it!
Originally tweeted by Dr Dan Goyal (@danielgoyal) on 01/03/2022.





